Heart failure is a clinical syndrome characterized by systemic perfusion inadequate to meet the body’s metabolic demands as a result of impaired cardiac pump function. This may be further subdivided into systolic or diastolic heart failure. In systolic heart failure, there is reduced cardiac contractility, whereas in diastolic heart failure there is impaired cardiac relaxation and abnormal ventricular filling.
The most common cause of heart failure is left ventricular (LV) systolic dysfunction (about 60% of patients). In this category, most cases are a result of end-stage coronary artery disease, either with a history of myocardial infarction or with a chronically underperfused, yet viable, myocardium. In many patients, both processes are present simultaneously. Other common causes of LV systolic dysfunction include idiopathic dilated cardiomyopathy, valvular heart disease, hypertensive heart disease, toxin-induced cardiomyopathies (e.g., doxorubicin, herceptin, alcohol), and congenital heart disease.
Right ventricular systolic dysfunction is usually a consequence of LV systolic dysfunction. It can also develop as a result of right ventricular infarction, pulmonary hypertension, chronic severe tricuspid regurgitation, or arrhythmogenic right ventricular dysplasia. A less-common cause of heart failure is high-output failure caused by thyrotoxicosis, arteriovenous fistulae, Paget’s disease, pregnancy, or severe chronic anemia.
Diastolic LV dysfunction (impaired relaxation) usually is related to chronic hypertension or ischemic heart disease. Other causes include restrictive, infiltrative, and hypertrophic cardiomyopathies. Inadequate filling of the right ventricle can result from pericardial constriction or cardiac tamponade.
Prevalence and Risk Factors
Heart failure is a common syndrome, especially in older adults. Although more patients survive acute myocardial infarction because of reperfusion therapy, most have at least some residual LV systolic dysfunction, which can lead to heart failure. Currently, 5.7 million Americans are afflicted with heart failure, approximately 2% of the population.1 Patients with heart failure account for about 1 million hospital admissions annually, and another 2 million patients have heart failure as a secondary diagnosis. Many of these patients are readmitted within 90 days for recurrent decompensation.
Patients at high risk for developing heart failure are those with hypertension, coronary artery disease, diabetes mellitus, family history of cardiomyopathy, use of cardiotoxins, and obesity.
Pathophysiology and Natural History
Although much progress has been made in the treatment of heart failure, there is a high overall annual mortality (5% to 20%), particularly in patients with New York Heart Association (NYHA) Class IV symptoms.2 Many patients succumb to progressive pump failure and congestion, although one half die from sudden cardiac death. Some patients die from end-organ failure resulting from inadequate systemic organ perfusion, particularly to the kidneys. Indicators of poor cardiac prognosis include renal dysfunction, cachexia, valvular regurgitation, ventricular arrhythmias, higher NYHA heart failure class, lower LV ejection fraction (LVEF), high catecholamine and B-type natriuretic peptide (BNP) levels, low serum sodium level, hypocholesterolemia, and marked LV dilation. Patients with combined systolic and diastolic LV dysfunction also have a worse prognosis than patients with either in isolation.
In LV systolic dysfunction, the body activates several neurohormonal pathways to increase circulating blood volume. The sympathetic nervous system increases heart rate and contractility, causes arteriolar vasoconstriction in nonessential vascular beds, and stimulates secretion of renin from the juxtaglomerular apparatus of the kidney. Unfortunately, catecholamines aggravate ischemia, potentiate arrhythmias, promote cardiac remodeling, and are directly toxic to myocytes. Stimulation of the renin-angiotensin system as a result of increased sympathetic stimulation and decreased renal perfusion results in further arteriolar vasoconstriction, sodium and water retention, and release of aldosterone. An increased aldosterone level, in turn, leads to sodium and water retention, endothelial dysfunction, and organ fibrosis.
In heart failure, baroreceptor and osmotic stimuli lead to vasopressin release from the hypothalamus, causing reabsorption of water in the renal collecting duct. Although these neurohormonal pathways initially are compensatory and beneficial, eventually they are deleterious, and neurohormonal modulation is the basis for modern medical treatment of heart failure.
In contrast, natriuretic peptides are hormones released by secretory granules in cardiac myocytes in response to myocardial stretching. They have a beneficial influence in heart failure, including systemic and pulmonary vasodilation, possible enhancement of sodium and water excretion, and suppression of other neurohormones.
With continuous neurohormonal stimulation, the left ventricle undergoes remodeling consisting of LV dilation and hypertrophy, such that stroke volume is increased without an actual increase in EF. This is achieved by myocyte hypertrophy and elongation. LV chamber dilation causes increased wall tension, worsens subendocardial myocardial perfusion, and can provoke ischemia in patients with coronary atherosclerosis. Furthermore, dilation of the LV chamber can cause mitral annular dilatation and functional mitral regurgitation, leading to pulmonary congestion.
In diastolic dysfunction, the primary abnormality is impaired LV relaxation, causing high diastolic pressures and poor filling of the ventricle. To increase diastolic filling, left atrial and pulmonary capillary pressures increase and pulmonary edema ensues. As a result, patients are often symptomatic with exertion when increased heart rate reduces LV filling time and circulating catecholamines worsen diastolic dysfunction. LV filling may also be very dependent on normal left atrial function. The loss of atrial function, as occurs with atrial fibrillation, may lead to a sudden worsening of LV filling and pulmonary congestion.
The American College of Cardiology (ACC) and American Heart Association (AHA) have developed a classification of heart failure based on stages of the syndrome. Stage A includes patients who are at risk for developing heart failure but who have no structural heart disease at present. The management strategy in this group is prevention of heart failure. Stage B includes patients with structural heart disease but no symptoms. The management goal is prevention of further LV remodeling leading to heart failure and the promotion of LV reverse remodeling. Stage C includes patients with structural heart disease with current or prior symptomatic heart failure. Diuretics, digoxin, and aldosterone antagonists may be added to angiotensin-converting enzyme (ACE) inhibitors and beta blockers, depending on the severity of symptoms. Cardiac resynchronization therapy (CRT) also may be considered. Stage D includes patients with severe refractory heart failure. Physicians should consider either end-of-life care or high-technology therapies such as cardiac transplantation or mechanical circulatory support, based on individual cases.
Table 1: American College of Cardiology–American Heart Association Classification of Chronic Heart Failure
| Stage | Description |
|---|---|
| A: High risk for developing heart failure | Hypertension, diabetes mellitus, CAD, family history of cardiomyopathy |
| B: Asymptomatic heart failure | Previous MI, LV dysfunction, valvular heart disease |
| C: Symptomatic heart failure | Structural heart disease, dyspnea and fatigue, impaired exercise tolerance |
| D: Refractory end-stage heart failure | Marked symptoms at rest despite maximal medical therapy |
CAD, coronary artery disease; LV, left ventricular; MI, myocardial infarction.
Signs and Symptoms
There is a wide spectrum of potential clinical manifestations of heart failure. Most patients have signs and symptoms of fluid overload and pulmonary congestion, including dyspnea, orthopnea, and paroxysmal nocturnal dyspnea. Patients with right ventricular failure have jugular venous distention, peripheral edema, hepatosplenomegaly, and ascites. Others, however, do not have congestive symptoms but have signs and symptoms of low cardiac output, including fatigue, effort intolerance, cachexia, and renal hypoperfusion. The NYHA functional classification scheme is used to assess the severity of functional limitations and correlates fairly well with prognosis.
Table 2: New York Heart Association (NYHA) Heart Failure Symptom Classification System
| NYHA Class | Level of Impairment |
|---|---|
| I | No symptom limitation with ordinary physical activity |
| II | Ordinary physical activity somewhat limited by dyspnea (e.g., long-distance walking, climbing two flights of stairs) |
| III | Exercise limited by dyspnea with moderate workload (e.g., short-distance walking, climbing one flight of stairs) |
| IV | Dyspnea at rest or with very little exertion |
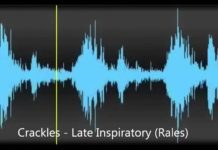
On physical examination, patients with decompensated heart failure may be tachycardic and tachypneic, with bilateral inspiratory rales, jugular venous distention, and edema. They often are pale and diaphoretic. The first heart sound usually is relatively soft if the patient is not tachycardic. An S3 and often an S4 gallop will be present. Murmurs of mitral or tricuspid regurgitation may be heard. Paradoxical splitting of S2 may be present because of delayed mechanical or electrical activation of the left ventricle. Patients with compensated heart failure will likely have clear lungs but a displaced cardiac apex. Patients with decompensated diastolic dysfunction usually have a loud S4 (which may be palpable), rales, and often systemic hypertension.
Diagnosis
The initial evaluation of new-onset heart failure should include an electrocardiogram, chest radiograph, and BNP assay. EKG findings of LV hypertrophy, left bundle branch block, intraventricular conduction delay, and nonspecific ST-segment and T wave changes support a diagnosis of heart failure. Q waves in contiguous leads strongly implicate a previous myocardial infarction and coronary artery disease as the cause. Chest radiographic findings of heart failure include cardiomegaly, pulmonary vascular redistribution, pulmonary venous congestion, Kerley B lines, alveolar edema, and pleural effusions.
The single most useful diagnostic test is the echocardiogram, which can distinguish between systolic and diastolic dysfunction. If systolic dysfunction is present, regional wall motion abnormalities or LV aneurysm suggest an ischemic basis for heart failure, whereas global dysfunction suggests a nonischemic cause. Echocardiography is helpful in determining other causes, such as valvular heart disease, cardiac tamponade, or pericardial constriction, and provides useful clues about infiltrative and restrictive cardiomyopathies. Echocardiography can also provide meaningful prognostic information about diastolic function, severity of hypertrophy, chamber size, and valvular abnormalities. In many cases, however, the exact cause of the heart failure cannot be discerned from the echocardiogram.
Cardiac catheterization can detect coronary atherosclerosis as the cause of heart failure. Severe coronary artery disease is so prevalent that coronary angiography routinely should be performed to exclude this cause and, if found, should lead to an assessment of myocardial viability, with a goal of revascularization. Coronary computed tomographic angiography or radionuclide myocardial imaging might also be suitable alternatives to exclude coronary artery disease in select patients.
Magnetic resonance imaging is useful in assessing for arrhythmogenic right ventricular dysplasia, myocardial viability, and infiltrative cardiomyopathies.
Objective information about functional capacity can be obtained from metabolic (cardiopulmonary) exercise testing. This test can distinguish ventilatory from cardiac limitations in patients with exertional dyspnea. A peak oxygen consumption or VO2max higher than 25 mL/kg/min is normal for middle-age adults, but a value lower than 14 mL/kg/min indicates severe cardiac limitation and poor prognosis.
A useful diagnostic test for the detection of heart failure is the BNP assay.6,7 BNP levels correlate with severity of heart failure and decrease as a patient reaches a compensated state. This blood test may be useful for distinguishing heart failure from pulmonary disease. Because smokers often have both these clinical diagnoses, differentiating between them may be challenging.
The routine use of invasive hemodynamic monitoring to guide the management of decompensated heart failure has not proved to be beneficial. However, invasive hemodynamic monitoring may be warranted if the diagnosis is uncertain, if the patient fails to respond to therapy, or if advanced therapies (heart transplant or mechanical circulatory support) are being considered.